
What is Teleaudiology?
More than ever, patients are becoming open to telehealth options. Telemedicine and teleaudiology are becoming more readily available with widespread advances in technology. This can improve your access to patients, keep costs in check, and improve efficiency in many areas of your practice. GSI has a store and forward solution through our proprietary automated audiometry solution, GSI AMTAS. Store and forward does not need direct supervision by the clinician and can be run by a trained staff member.
Interested in teleaudiology? View our Q&A below about the development, benefits, and validation. Additionally, you can download a PDF copy of these questions and find other educational resources on this topic.
The US Congress has defined four different types of telemedicine*. First is Synchronous, a live video or face-to-face appointment with a healthcare provider in one location and the patient in a separate location. Second, Asynchronous, or store and forward, which is when the data is collected without a healthcare professional or licensed provider present, and the results are then forwarded to the licensed provider for interpretation. The third type of telemedicine is remote patient monitoring, in which data is collected for monitoring a chronic illness or a chronic disease that will then be transmitted back to another location for interpretation. And finally there is mobile health, which is a clinic in a portable environment, such as a truck. Clinicians have all the tools they need to perform the medical evaluation and bring the office to the patient.
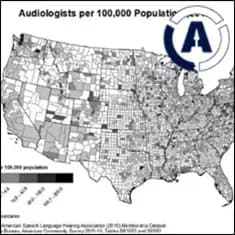
There is a growing need for telemedicine in all sectors of healthcare, including audiology. The demand for hearing healthcare outweighs audiologic testing capabilities. It has been projected that there will be a shortfall of providers for hearing healthcare services. In addition to the lack of hearing healthcare providers, the aging population is growing substantially, and patients are finding it more and more difficult to get access to hearing healthcare in a timely or convenient manner. There is also an increased focus on testing at a distance with limited physical exposure to protect patients and providers.
It is important to address this widening gap in the delivery of hearing healthcare. Ideally, an increase of hearing healthcare providers would allow for more access to hearing healthcare; however, projections indicate that audiology is a flat or shrinking profession. Improving access and increasing productivity by incorporating teleaudiology is the most viable solution to this dilemma.
Teleaudiology is not new; however, audiologists are beginning to recognize the importance of reaching patients regardless of the barriers we face such as distance, a lack of providers, and not enough time.
*Congressional Research Service. “Telehealth and Telemedicine: Frequently Asked Questions.” 2020. PDF file.
There is no better time to implement some level of teleaudiology than now. Teleaudiology has been growing in availability for the past several years, with the aging population growing at a record pace and the number of audiologists staying essentially the same. Advancements in diagnostic audiology and therapeutic technologies combined with readily available communication methods have provided an opportunity to revolutionize access to hearing health services in low resource areas across the globe.
Teleaudiology can lessen the burden faced by patients and providers. It is a way to potentially shorten travel distance, decrease wait time for and at the appointment, and receive a quality basic hearing assessment when it may not have otherwise been available. For hearing healthcare providers, this is a way of increasing efficiency. There are a variety of other tasks that may be attended to while utilizing certain methods of teleaudiology, and when direct supervision is not necessary, an audiologist may not have to even be on-site if they have a properly trained staff.
There are two main ways to perform teleaudiology. Synchronous, or live face-to-face, and Asynchronous, or store and forward.
Synchronous is typically what people think of when they imagine telemedicine. It requires a video connection between the audiologist and the patient. A technician or an audiology assistant is required at the patient site to be the audiologist’s “hands.” Synchronous teleaudiology is similar to a live appointment in the sense that the audiologist is present and facilitating the appointment.
The equipment used for synchronous teleaudiology must be PC-based and paired with a two-way video stream. The audiologist controls the equipment from their office while the patient and the technician are in a different location. Audiometry, hearing aid fittings, and counseling can be performed this way. With an experienced and trained technician, video otoscopy and REM may also be utilized.
Synchronous Requirements:
- Personnel Requirements
a. Audiologist in one office
b. Trained technician in the other office with patient - Technology Requirements
a. High Speed internet connection to support video conference
b. Reliable power for equipment
Asynchronous is a store and forward technology that captures data remotely, stores results, and forwards them to an audiologist for interpretation. This type of teleaudiology does not require an audiologist to be present for the evaluation, and it is more limited in the types of tests that can be performed. The patient interacts with a trained technician to obtain information that is then forwarded to an audiologist for interpretation, recommendations, and next steps.
Asynchronous Requirements:
- Personnel Requirements
a. Technician to place transducers on patient and forward results
b. Audiologist to interpret results as scheduling permits - Technology Requirements
a. Reliable power for equipment
b. Internet for transmission of results
AMTAS is a patient-directed evaluation tool that uses patented test methods and accuracy algorithms to perform diagnostic or screening audiometry. AMTAS was created as a resource for clinicians to help manage their busy schedules and promote an efficient office environment. With over 15 years of research and development, the validity of AMTAS has been proven through comprehensive studies to set it apart from its competitors.
AMTAS Testing:
-
AMTAS Pro offers diagnostic air conduction, bone conduction, and speech (SRT and WRS) testing with masking. This self-directed test typically takes about 15 minutes to complete and the report provides nine quality indicators to assist the clinician in determining the accuracy of the test. AMTAS Pro is operated through a PC connected to a compatible GSI audiometer.
-
AMTAS Flex is tablet-based and does not require an audiometer. This version offers air conduction screening and threshold audiometry. The screening test typically takes 1 - 2 minutes to complete and displays a Pass or Refer at the completion of the test. The threshold test provides six quality indicators and the AMCLASS audiogram classification.
The results of AMTAS are data driven and evidence based. Patient responses are used to calculate the overall accuracy and a number of other important markers called quality indicators that will provide the audiologist with the necessary information for interpretation.
These patented quality indicators provide information about the patient’s behavior during testing. Using these provides the clinician insight on how to proceed with counseling and further testing. The quality indicators are as follows:
- Predicted Accuracy - Overall Quality: Good, Fair, Poor. Based on the quality indicators. ’
- Predicted Average Absolute Difference - Difference between automated and manual thresholds based on a study where five expert audiologists tested patients manually and compared the results to AMTAS evaluations. Based on research, see AMTAS Validations Publications later in this document.
- Masker Alerts - These indicate thresholds where masking may have been too high or too low.
- Time Per Trial - Measures the average time from stimulus to patient response.
- False Alarm Rate - The number of times the patient responded with no stimulus presented is divided by number of trials when no stimulus was presented. When there is a false alarm, AMTAS displays a message to alert the patient that they responded yes when there was not a tone presented.
- Average Test-Retest Difference - Displays the average difference between 1 kHz test and retest in the right and left ears.
- Quality Check Fail Rate -When threshold is established, AMTAS presents a stimulus that is 5 dB above threshold. The patient should hear this tone. QC fail indicated the number of times patient did not respond to stimulus above threshold divided by the number of measured thresholds. If this is high, it can indicate malingering or that the patient is not a good candidate for AMTAS.
- Number of Air/Bone Gap > 35 dB - This is the number of air/bone gaps that exceed 35 dB.
- Number of Air/Bone Gap < -10 dB - This is the number of air/bone gaps that are less than 10 dB.
Every audiologist seeing patients can benefit from implementing AMTAS. There are several tasks that an audiologist can attend to while a patient is working through AMTAS, such as seeing other patients or performing other tests that require the skills of an audiologist. Since direct supervision is not necessary, an audiologist does not have to be on-site if they have a properly trained staff. By saving the time spent doing basic audiologic testing, the audiologist has an opportunity to be more efficient.
Current examples of the use of GSI AMTAS:
-
If an ENT physician does not have an audiologist on staff, the patient is referred to a local audiologist for evaluation. The patient then returns to the ENT for treatment. This results in three appointments and possibly multiple co-pays. If the ENT had utilized AMTAS, they would still likely refer to audiology, but they would be able to complete the patient’s appointment more efficiently.
-
If an audiologist is supporting an ENT clinic and has several patients who need audiometry at the same time, the patients must wait until the audiologist becomes available before they can be seen. This can lead to long wait times for a hearing test. If AMTAS was available, more than one patient could be evaluated simultaneously.
-
If a busy clinic has AMTAS, a walk-in patient with sudden hearing loss can be tested immediately and worked into the schedule for same day treatment.
-
A satellite office where an audiologist is not available every day can see more patients and be more effective by using AMTAS. The testing results can be forwarded to the audiologist for review.
The simple answer is both! The most ideal teleaudiology program includes elements of both store and forward and live teleaudiology. For the patient, store and forward will increase access to audiology services. The patient does not have to be fit into a busy audiologist’s schedule for a hearing test which allows for fast and more flexible accommodations. Live teleaudiology gives the patient the flexibility to be “seen” from a distance and at a mutually convenient time for counseling, follow up, and additional testing.
Teleaudiology allows audiologists to be more efficient. Using a combination of store and forward and live teleaudiology allows audiologists to be more purposeful with their schedules. Store and forward reduces time spent on routine testing and gives audiologists an opportunity to spend more time providing meaningful services that require more audiologic expertise.
Synchronous and Asynchronous Teleaudiology can be combined to provide patients with outstanding hearing healthcare regardless of distance or time constraints. It is important to start with a detailed plan of action. Determine which pieces of teleaudiology you are able to access immediately and which ones will require training and acquisition of equipment.
Interested in asynchronous teleaudiology? Below is a list of equipment requirements for AMTAS.
AMTAS Pro
- Software system integrated with a GSI audiometer (the AudioStar Pro or Pello) that is capable of capturing threshold AC and BC (masked) as well as forced-choice SRT and WRS.
- Utilizes DD450 headphones (commonly used for full frequency testing) and a forehead bone placement.
AMTAS Flex
- Tablet-based software that can perform simple four frequency screenings and threshold AC (masked).
- Utilizes specially designed DD450 headphones that plug into USB.
In addition, below are some ideas of ways to implement synchronous teleaudiology.
- Video Chat Check in – use FaceTime, Skype, or Zoom (or other video conferencing services) to “see” how your patients are doing. See if there is anything you can help walk them through via video.
- Utilize hearing aid mobile apps to adjust hearing aids remotely.
- Contact your local equipment distributor to determine what is needed for synchronous teleaudiology.
Yes! You can find a list of validation publications below.
- Margolis, R.H. Automated Audiometry - Progress or Pariah? Audiology Online www.audiologyonline.com/articles. January 17, 2005.
- Margolis, R.H. Automated Audiometry: Progress or Pariah. Audiology Today 17:21, 2005. •Margolis, R.H., Saly, G., Le, C., Laurence, J. Qualind™: A Method for Assessing the Accuracy of Automated Tests. J. Amer. Acad. Audiol., 18, 78-89, 2007 .
- Margolis, R.H., Saly, G.S. Toward a standard description of hearing loss. Int. J. Audiology 46, 746-758, 2007.
- Margolis, R.H., Morgan, D.E. The Value of Automated Audiometry. Insights in Practice for Clinical Audiology, January 2008.
- Margolis, R.H., Saly, G.L. Prevalence of hearing loss types in a clinical population. Ear and Hearing, 29, 524-532, 2008.
- Margolis, R.H., Saly, G.L. Toward a standard description of hearing loss. Int. J. Audiology, 46, 746-758, 2007.
- Margolis, R.H., Saly, G.L. Asymmetrical Hearing Loss: Definition, Validation, Prevalence. Otology & Neurotology, 29, 422-431, 2008.
- Margolis, R.H., Morgan D.E. Automated Pure-Tone Audiometry - An Analysis of Capacity, Need, and Benefit. Amer. J. of Audiology, 17, 109113, 2008.
- Margolis, R.H., Glasberg, B.R., Creeke, S., Moore, B.C.J. AMTAS Automated Method for Testing Auditory Sensitivity: Validation Studies. Int. J. Audiology,49, 185-194, 2010.
- Margolis, R.H., Frisina, R., Walton, J.P. (2011). Automated method for testing auditory sensitivity: II. Air Conduction Audiograms in Children and Adults. Int J Audiology, 50, 434-439, 2011.
- Margolis, R.H., Moore, B.C.J. Automated method for testing auditory sensitivity: III. Sensorineural hearing loss and air-bone gaps. Int J Audiology, 50, 440-447, 2011.
- Margolis, R.H., Eikelboom, R.H., Johnson, C., Ginter, S.M., Swanepoel, D.W., Moore, B.C.J. False Air-Bone Gaps at 4 kHz in Listeners with Normal Hearing and Sensorineural Hearing Loss. Int. J. Audiology 52:526-532, 2013.
- Margolis, R.H., Wilson, R.H., Popelka, G.R., Eikelboom, R.H., Swanepoel, D.W. Distribution characteristics of normal pure-tone thresholds. J. Audiology, 54, 796-805, 2015.
- Margolis, R.H., Wilson, R.H., Popelka, G.R., Eikelboom, R.H., Swanepoel, D.W. Distribution Characteristics of Air-Bone Gaps: Evidence of Bias in Pure-Tone Audiometry. Ear & Hearing, 37, 177-188, 2016.
- Margolis, R.H., Killion, M,C, Bratt, G.W., Saly, G.L. Validation of the Home Hearing Test. J Amer. Acad. Audiol., 27, 416-420, 2016
Additional Resources
Check out our educational resources below when considering teleaudiology for your practice. We have an informative webinar on how to improve access to hearing healthcare and a podcast reviewing what’s available in the market today - live, video, face to face, and our store and forward option. We also have included direct links below from some of our ask the experts on teleaudiology.
Email us at audiology@grason-stadler.com with any inquires.
Teleaudiology Webinar
Teleaudiology: Improving Access to Hearing Healthcare
Audiology Online course, subscription required for CEU credit.
Learning Level: Introductory
Presenter: Laura Prigge, AuD
Advancements in audiology diagnostic and therapeutic technologies combined with readily available communication technologies have provided an opportunity to revolutionize hearing health services in low-resource communities across the globe. This presentation will define modalities of teleaudiology and demonstrate how each method can be applied to bridge the gap to quality hearing health services.
Teleaudiology Ask the Experts
SYNCHRONOUS VS ASYNCHRONOUS?
WHO BENEFITS FROM AMTAS?
WHAT GSI EQUIPMENT IS TELEPRACTICE FRIENDLY?