Patient Checklist - The Basics of Tympanometry


This blog entry was written as a patient-focused overview about what to expect during tympanometry testing. We encourage you to share this with your patients if they have questions about the process and benefits of the test or use it as a guide when talking with your patients before the testing begins. It’s crucial that every patient that walks through a clinician’s office doors not only feels comfortable, but also understands the basics of their visit.
Tympanometry is a valuable diagnostic tool used by healthcare professionals to assess the wellbeing of the middle ear. It’s a non-invasive and painless way for clinicians to obtain essential information about the middle ear’s function by measuring the eardrum movement with a pressure sweep.
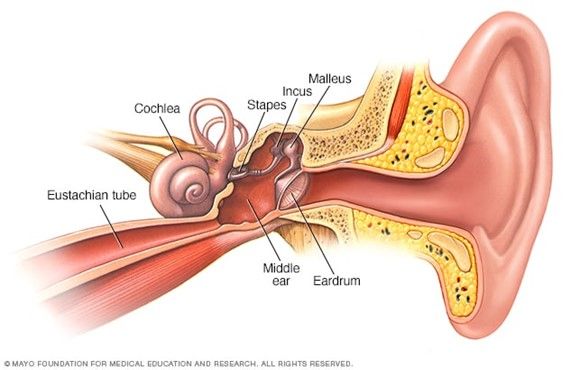
Image credit: Mayo Clinic
The middle ear lies behind the eardrum and is composed of three small bones: the malleus (hammer), the incus (anvil), and the stapes (stirrup). These bones vibrate when soundwaves hit the eardrum and transmit the message to the inner ear.
A tympanometer is the tool that healthcare professionals use to conduct the test. After otoscopy, the probe from the specialized instrument is inserted into the ear canal and generates changes in air pressure. The tympanometer records the responses of the eardrum and the results are evaluated by the healthcare professional.
The hearing healthcare professional will perform a preliminary exam called an otoscopy. This allows audiologists to look inside of the ear with a lighted and magnified lens to observe the ear canal, eardrum, and other aspects of the middle ear.

When the tympanometry testing starts, the patient will have a small probe placed in their ear in order to create a seal of the ear canal. The patient will then hear a low pitched tone and feel a slight, painless pressure sensation in their ear. This has been described as similar to the feeling you get in your ears before they “pop” when you are on an airplane.
One of the primary reasons tympanometry is essential is its ability to detect middle ear disorders. Conditions like Eustachian tube dysfunction and otosclerosis can cause significant discomfort and even hearing loss. But with the assistance of tympanometry, these issues can be identified quickly and efficiently to ensure treatment is introduced to the patient early on.
After the test is complete, the healthcare professional will review the results of the tympanometry test, which is called a tympanogram. The tympanogram will give the audiologist an indication of if the patient’s middle ear is functioning properly or if there is an issue such as fluid build-up, blockage, or a hole in the eardrum. The audiologist will conduct additional tests depending on the results from the tympanogram.

Tympanometry also plays a vital role in the fitting and management of hearing aids. Before a healthcare professional typically recommends hearing aids, audiologists need to assess the middle ear’s health to ensure the device will function properly. As they assess the middle ear, they are looking for any issues that may impact the effectiveness of the hearing aid, such as fluid accumulation or stiffness in the middle ear. It also helps determine the appropriate setting for their hearing aids, as this setting is unique to each patient.
Tympanometry is a critical component of audiological evaluations, which is why it’s crucial our patients understand the basics. The ability to closely assess the middle ear function and detect disorders early on makes tympanometry a valuable diagnostic tool for all patients, no matter their age. From diagnosing middle ear disorders to assisting in hearing aid fittings, tympanometry plays a pivotal role in hearing healthcare all around the world.
Laura Prigge, AuD is the Manager of Clinical Education and Training at GSI. Laura received her Doctorate of Audiology degree from AT Still University, a Master’s of Arts in Audiology from UCONN and a Bachelor’s of Science degree in Communication Disorders from Western Illinois University. Laura’s 20+ years of experience includes providing manufacturing support for a leading hearing aid manufacturer as well as technical audiology training and support for an international audiologic equipment company. Prior to that, she managed education and training at another hearing aid manufacturer and conducted audiologic evaluations on children, adults, and geriatric patients at a retail hearing center.